An Achilles Tendon Rupture How Would I Know I Suffered It?
Overview
 A tendon is a band of tissue that connects a muscle to a bone. The Achilles tendon runs down the back of the lower leg and connects the calf muscle to the heel bone. Also called the ?heel cord,? the Achilles tendon facilitates walking by helping to raise the heel off the ground. The Achilles tendon is at the back of the heel. It can be ruptured by sudden force on the foot or ankle. If your Achilles tendon is ruptured you will be unable to stand on tiptoe, and will have a flat-footed walk. It is important to diagnose and treat this injury as soon as possible, to help promote healing. Treatment involves wearing a plaster cast or brace (orthosis) for several weeks, and possibly having an operation.
A tendon is a band of tissue that connects a muscle to a bone. The Achilles tendon runs down the back of the lower leg and connects the calf muscle to the heel bone. Also called the ?heel cord,? the Achilles tendon facilitates walking by helping to raise the heel off the ground. The Achilles tendon is at the back of the heel. It can be ruptured by sudden force on the foot or ankle. If your Achilles tendon is ruptured you will be unable to stand on tiptoe, and will have a flat-footed walk. It is important to diagnose and treat this injury as soon as possible, to help promote healing. Treatment involves wearing a plaster cast or brace (orthosis) for several weeks, and possibly having an operation.
Causes
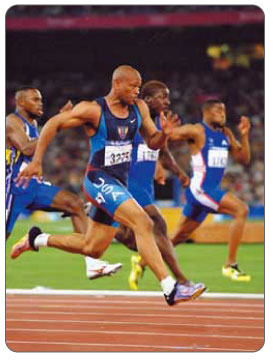
Your Achilles tendon helps you point your foot downward, rise on your toes and push off your foot as you walk. You rely on it virtually every time you move your foot. Rupture usually occurs in the section of the tendon located within 2 1/2 inches (about 6 centimeters) of the point where it attaches to the heel bone. This section may be predisposed to rupture because it gets less blood flow, which also may impair its ability to heal. Ruptures often are caused by a sudden increase in the amount of stress on your Achilles tendon. Common examples include increasing the intensity of sports participation, especially in sports that involve jumping, falling from a height, stepping into a hole.
Symptoms
Often the person feels a whip-like blow that is followed by weakness in the affected leg - usually he or she is not able to walk afterwards. At place where the tendon ruptured, a significant dent is palpable. Often the experienced physician can diagnose a ruptured Achilles tendon by way of clinical examination and special function tests. Imaging techniques, such as ultrasound and magnetic resonance imaging (MRI) allow for a more precise diagnosis.
Diagnosis
Diagnosis of Achilles tendon rupture is not difficult. Usually, the diagnosis is obvious after examination of the ankle and performing some easy foot maneuvers (such as attempting to stand on the toes). When an Achilles tendon rupture occurs, there is often clinical confirmation of tenderness and bruising around the heel. A gap is felt when the finger is passed over the heel area, where the rupture has developed. All individuals with a full-blown rupture of the tendon are unable to stand on their toes. There is no blood work required in making a diagnosis of Achilles tendon rupture. The following are three common radiological tests to make a diagnosis of Achilles tendon rupture. Plain X-rays of the foot may reveal swelling of the soft tissues around the ankle, other bone injury, or tendon calcification. Ultrasound is the next most commonly ordered test to document the injury and size of the tear. For a partial tear of the Achilles tendon, the diagnosis is not always obvious on a physical exam and hence an ultrasound is ordered. This painless procedure can make a diagnosis of partial/full Achilles tendon rupture rapidly. Ultrasound is a relatively inexpensive, fast, and reliable test. MRI is often ordered when diagnosis of tendon rupture is not obvious on ultrasound or a complex injury is suspected. MRI is an excellent imaging test to assess for presence of any soft-tissue trauma or fluid collection. More importantly, MRI can help detect presence of tendon thickening, bursitis, and partial tendon rupture. However, MRI is expensive and is not useful if there is any bone damage.
Non Surgical Treatment
As debilitating as they can be, the good news is that minor to moderate Achilles tendon injuries should heal on their own. You just need to give them time. To speed the healing, you can try the following. Rest your leg. Avoid putting weight on your leg as best you can. You may need crutches. Ice your leg. To reduce pain and swelling, ice your injury for 20 to 30 minutes, every three to four hours for two to three days, or until the pain is gone. Compress your leg. Use an elastic bandage around the lower leg and ankle to keep down swelling. Elevate your leg. Prop you leg up on a pillow when you're sitting or lying down. Take anti-inflammatory painkillers. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) and naproxen (Aleve) will help with pain and swelling. However, these drugs have side effects, such as an increased risk of bleeding and ulcers. They should be used only occasionally unless your health care provider says otherwise and should be taken with food. Check with your doctor before taking these if you have any allergies, medical problems or take any other medication. Use a heel lift. Your health care provider may recommend that you wear an insert in your shoe while you recover. It will help protect your Achilles tendon from further stretching. Practice stretching and strengthening exercises as recommended by your health care provider. Usually, these techniques will do the trick. But in severe cases of Achilles tendon injury, you may need a cast for six to 10 weeks or even surgery to repair the tendon or remove excess tissue. 
Surgical Treatment
Immediate surgical repair of the tendon is indicated in complete tears. Delaying surgery can lead to shortening of the tendon, formation of scar tissue and decreased blood flow, which can lead to a poor outcome. Following surgery your ankle will be put in an immobilizing device and you will be instructed to use crutches to limit weight bearing and protect the joint. Over the next 2-4 weeks weight bearing will be increased and physical therapy will be initiated. The surgeon will determine the physical therapy timeline and program. Physical Therapy, Treatment will emphasize gradual weaning off the immobilizing device, increased weight bearing, restoration of ankle range of motion and strengthening of the lower leg muscles. It is important that the physician and therapist communicate during the early stages and progress your program based on the principles of healing so as not to compromise the Achilles tendon. Patient will be progressed to more functional activities as normal ankle range of motion and strength is restored.